Complete list of POC grants secured by UNeMed at the University of Nebraska Medical Center and the University of Nebraska at Omaha.
Tumor-targeted drugs for prostate cancer imaging and molecular radiotherapy
Approved: Oct. 10, 2011
Amount: $172,839
Principal Investigator: Janina Baranowska-Kortylewicz, PhD
Summary: Novel radiopharmaceutical compound targeting specific cancer cells for the better treatment, diagnosis and tracking of tumors in the prostate, breast and ovaries. Such a targeted approach is expected to dramatically reduce harmful side-effects while improving treatment effectiveness.
Outcome: Funds used to complete all pre-clinical studies, and allowed the successful submission of an Investigative New Drug application to the FDA, which would allow a phase one clinical trial in prostate cancer patients. The clear path to a clinical trial attracted an entrepreneur from Kansas City who created a startup company, Calidum Inc., with an exclusive license for the technology. Calidum is currently raising funds to support the clinical trial.
Dentotropic mouthwash formulation for the prevention and treatment of dental caries and periodontal diseases
Approved: Feb. 2, 2012
Amount: $243,000
Principal Investigator: Dong Wang, PhD
Summary: A new nanoparticle formulation for the treatment of oral diseases allows for extended and localized delivery that improves the effectiveness of existing drugs while reducing unwanted side-effects.
Outcome: Funds supported tests that showed apparent effectiveness of the compound. Further studies—including toxicity and stability—are required for further commercial development. Discussions with potential commercial partners are ongoing.
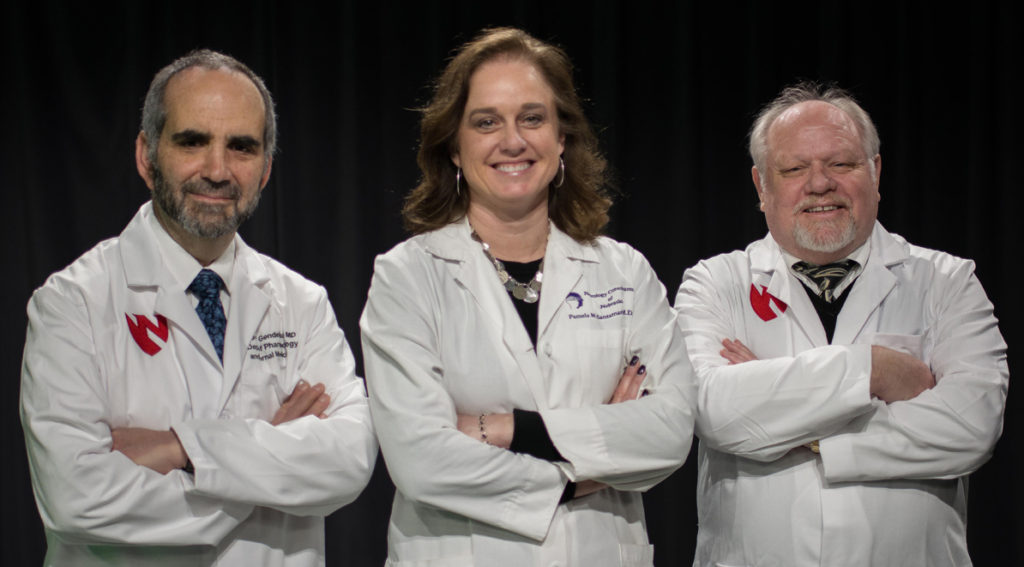
Immunoprotection for Parkinson’s disease
Approved: Nov. 1, 2013
Amount: $150,000
Principal Investigator: Howard Gendelman, M.D.
Summary: A vaccine strategy capable of slowing the progression of Parkinson’s disease
Outcome: Funds were used to support a clinical trial that explored one key component of the vaccine called an adjuvant. Tests showed the adjuvant alone was enough to transform the immune profile of Parkinson’s patients. More than $100,000 additional funds were provided by a major pharmaceutical company to further support the clinical trial, and discussions are underway to expand the tests in a larger groups of patients.
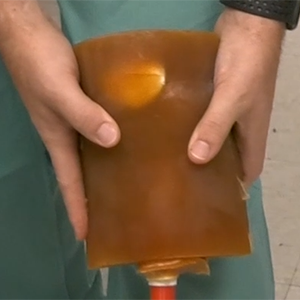
Resorbable stent to assist in arteriovenous fistula maturation
Approved: May 15, 2012
Amount: $85,000
Principal Investigator: Marius Florescu, M.D.
Summary: A new device that improves success rates for AV fistulas, a procedure that joins an artery and a vein for the purpose of creating a portal to be used in dialysis for patients with failing kidneys.
Outcome: Funds paid for first successful fistula creation in animals and led to an advanced prototype with several potential clinical partners expressing an interest in the final design. The research in now planning a new study with the improved prototype.
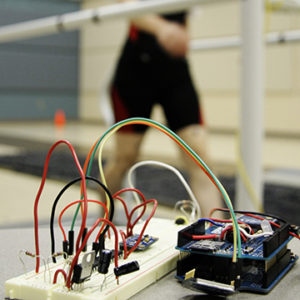
Use of gait analysis to assess the likelihood of falls in at-risk populations
Approved: Sept. 4, 2012
Amount: $82,500
Principal Investigator: Nick Stergiou, PhD
Summary: A system of sensors worn by a patient that can detect and record neuromuscular information. The information can then be analyzed to detect conditions such as Parkinson’s disease, peripheral artery disease, and the susceptibility of elderly patients to falls.
Outcome: Funds paid for a study of the device, and based on the positive results of the tests, a medical device company signed an agreement for exclusive rights to the underlying patents. They are currently working on applying for additional funding to support a clinical trial with a more advanced version of the prototype.
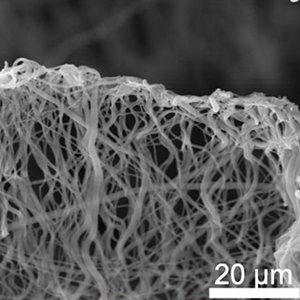
NanoART for preclinical safety assessment
Approved: March 1, 2013
Amount: $225,000
Principal Investigator: Howard Gendelman, M.D.
Summary: Funds helped test and develop novel long-acting nanoformulations for anti-HIV medications.
Outcome: Nanoformulations developed by this grant helped produced a partnership with a major pharmaceutical firm that has contributed more than $1.18 million in additional research funding. If previous studies are verified by an independent third party as expected, the collaboration would also expand to a much wider and deeper examination of the technology and its capabilities.
Novel antibodies for MUC4: applications in structure-functional analysis, and diagnosis and therapy of human cancers
Approved: May 1, 2013
Amount: $100,000
Principal Investigator: Surinder Batra, PhD
Summary: Measuring a protein called MUC4 could help improve and refine the diagnosis and treatment strategies of some type of cancers, including pancreatic, lung, breast, ovarian and cervical.
Outcome: Results from the studies led to the creation of a startup company, Sanguine Diagnostics. The studies paid for by the POC grant led to additional work support through NIH grants. Sanguine also built on the findings of the POC studies to secure two Small Business Technology Transfer grants from the federal government, totaling $525,000. Sanguine is planning additional studies as they work toward developing better tissue diagnostic tools.
ARRESS and Lock-Block
Approved: June 27, 2014
Amount: $250,000
Principal Investigator: Greg Gordon, M.D.
Summary: Devices are designed to protect healthcare providers from repeated radiation exposure while reducing strain and stress on a provider’s joints and muscles through improved ergonomics.
Outcome: Funds supported a study that provided documented proof of assumed advantages of new devices. Complaints of musco-skeletal injury, fatigue and injury were reduced for physicians using the system. Radiation exposure levels were also significantly reduced, while workflow in the operating room also improved. Radux, the startup company built on the innovations, used the data to attract investors, putting Radux on the fast-track to an expected product launch this spring.
Drug candidates for Paf1/PD2: A novel target to restrict its comprehensive role in drug resistance of pancreatic and ovarian cancer stem cells
Approved: March 1, 2014
Amount: $250,000
Principal Investigator: Surinder Batra, PhD
Summary: A protein associated with pancreatic cancer, pancreatic differentiation factor 2 or PD2, was identified as a key player in the development and recurrence of pancreatic and ovarian cancers.
Outcome: Funds supported a multi-campus collaboration that leveraged the super-computer at UNO’s Holland computing center to simulate potential drug candidates targeting PD2. After creating an accurate computer model of PD2, researchers successfully identified potential candidates. Based on those results, one pharmaceutical company has expressed a substantial interest in proposed follow-on studies, although additional funds are necessary to move forward.
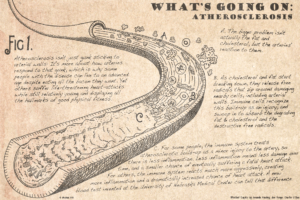
MAA-adduct isolation and identification of the adducted macromolecule (analyte)
Approved: July 1, 2014
Amount: $100,000
Principal Investigator: Geoffrey Thiele, PhD
Summary: A protein known as MAA, short for malondialdehyde-acetaldehyde, appears to differentiate between a relatively benign form of artery disease from a more lethal form that can result in a sudden and unexpected heart attack. Studies show a simple blood might be used to more accurately predict risk of the more dangerous variety of coronary artery disease.
Outcome: Funds paid for a study to develop a more accurate blood test. Five additional leads were developed in the study, which helped establish collaborative agreements with two commercial partners, including the creation of a new startup company, HealthCheck Diagnostics.
Improve Potency and oral bioavailability of the lead compound 13-197
Approved: Feb. 16, 2015
Amount: $250,000
Principal Investigator: Amarnath Natarajan, PhD
Summary: NF-kB signaling plays an important role in the development and progression of numerous diseases. A novel inhibitor of NF-kB, 13-197, had demonstrated potent anti-proliferative activity.
Outcome: Based on feedback from industry representatives, POC funds were used to develop more potent and drugable analogs of 13-197. All tests are not yet complete, but one pharmaceutical company has already expressed a strong interest in pursuing any new leads generated from the POC study.
PortCas
Approved: Nov. 1, 2015
Amount: $9,000
Principal Investigator: Joseph Siu, PhD
Summary: An ultralight laparoscopic simulator for the training of surgical residents that is a less expensive and portable.
Outcome: Funds supported the creation of a training program for laboratory personnel as the technology continues moving toward its first round of “alpha” testing later this year.
Novel pyrrolomycins as anti-anthrax and anti-MRSA agents
Approved: March 7, 2016
Amount: $250,000
Principal Investigator: Rongshi Li, PhD
Summary: A new compound showed great potential as a highly potent antibacterial agent against anthrax and methicillin-resistant Staphylococcus aureus, MRSA.
Outcome: Grant funded studies are still ongoing.
Reliability of portable device to measure respiration and step rates
Approved: March 7, 2016
Amount: $76,410
Principal Investigator: Jennifer Yentes, PhD
Summary: A new platform that measures the relationship between breathing and walking shows the potential to predict when chronic obstructive pulmonary disease, COPD, suddenly flares up into a potentially deadly episode known as an exacerbation.
Outcome: Funds supported a clinical test that produced an unexpected amount of data, which lead to an improved algorithm to interpret and process all the information. The POC results led to an improved version of the wearable device and second clinical study that will held at the University of Alabama-Birmingham and the University of Michigan.
Development and applications of quantifiable sympathetic vasomotion
Approved: Aug. 1, 2016
Amount: $200,052
Principal Investigator: Irving Zucker, PhD
Summary: A system for assessing the accuracy and effectiveness of renal denervation as an alternative treatment for high blood pressure.
Outcome: Studies are on-going. Based on earlier tests, a major medical device company is interested in the platform, and plans to visit campus later this year to review the results of the current study.
Pupillary examination using a simulated training model of the eye
Approved: Jan. 5, 2017
Amount: $80,636
Principal Investigator: Deepta Ghate, PhD
Summary: A virtual and augmented reality simulator for examining pupils and pupillary disorders. The simulator is designed to teach medical students, residents, and other health care professionals how give a proper pupil examination and properly diagnose various diseases.
Outcome: Grant allowed the creation of a collaborative licensing agreement with a major medical simulator company, which will develop the simulator and incorporate into their existing line of products.
Development of the Aquablade catheter for treatment of aortic dissection
Approved: Jan. 23, 2017
Amount: $210,000
Principal Investigator: Jason MacTaggart, M.D.
Summary: The Aquablade is a device that uses high-pressure water to cut tissue inside an artery or vein. It is initially being developed for the treatment of aortic dissections.
Outcome: Grant will focus on the development of a functional prototype through a collaboration with a medical device manufacturing group. Once the prototype is developed additional tests will be conducted in UNMC labs.
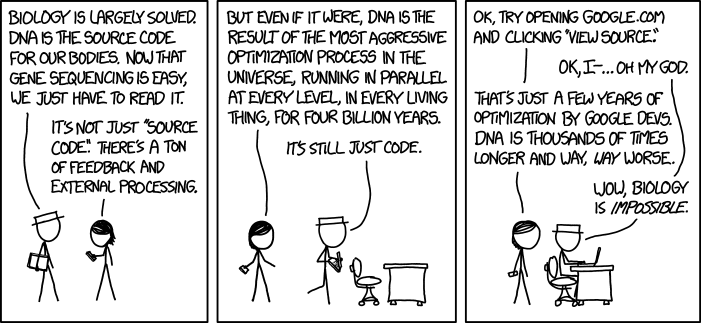




 I am now a Licensing Associate now at UNeMed Corporation, the technology transfer office at the University of Nebraska Medical Center. UNeMed gave me the opportunity to attend Association of University Technology Managers’ 2017 Annual Meeting in Hollywood, Fla. I noticed a stark difference in cultures between the two conferences.
I am now a Licensing Associate now at UNeMed Corporation, the technology transfer office at the University of Nebraska Medical Center. UNeMed gave me the opportunity to attend Association of University Technology Managers’ 2017 Annual Meeting in Hollywood, Fla. I noticed a stark difference in cultures between the two conferences.