Cats, pajamas & science will never be the same

UNMC researcher Sam Sanderson, PhD, checks the results of a recent quality control test at his Omaha lab. His startup company, Prommune, is based on an innovation he developed. (File Photo: Charlie Litton)
by Charlie Litton, UNeMed | Aug. 9, 2017
Not long ago, we had a very important discussion. We needed to understand what, exactly, are “cat’s pajamas.” Are they literally pajamas…that cats wear…to bed? Were footies in play? Who would want to put PJs on a cat? Why?
It was a deep dive into strange worlds of felines, sleep garments and, of course, the white-hot ball of fire that was Sam Sanderson.
Sanderson, a UNMC inventor who built a startup around his innovations, had just been in the office. He had an update for us those many weeks ago.
He just landed a huge grant that would further his research, and wanted to share the good news. He just needed to cross a few T’s, dot some I’s, and he’d be “cocked, locked and ready to rock.”
I don’t recall the exact context, but he did drop the “cat’s pajamas” on us at some point. He usually did. It was a verbal tic that grew into something of a catchphrase for Sam.
 “Sam was always quick with a ‘golly gee’ or a ‘gee wiz,'” said UNeMed President and CEO Michael Dixon. “I’m fairly certain I won’t be able to use the phrase ‘the cat’s pajamas’ without thinking of Sam.”
“Sam was always quick with a ‘golly gee’ or a ‘gee wiz,'” said UNeMed President and CEO Michael Dixon. “I’m fairly certain I won’t be able to use the phrase ‘the cat’s pajamas’ without thinking of Sam.”
Then Sam didn’t wake up Tuesday morning.
It’s a bitter pill that won’t wash down anytime soon. Yet, I can’t help but wonder what he might say about that.
I bet he’d call it a “bummer, man.”
Then I expect he’d shrug, and find some positive light to shine on it. That was his way too.
“If Sam caught you in the hallway, you were guaranteed to be late to your next meeting,” Dixon said. “But that was okay because his excitement and enthusiasm was infectious. I always left a meeting with Sam feeling better about myself and the world around me.”
I wouldn’t normally admit this, but Sam was my favorite of all UNMC’s talented inventors. It’s not that his innovations where necessarily any better than anyone else’s, although they were pretty great.
He had his own gravitational force. Once pulled in, you were infected and transformed. You walked away wanting to climb mountains.
More than that, you wanted him to summit his Everest. You rooted for him because he earned it. He put in the time. He never gave up, even when no one else seemed to believe in him.
He fought long and hard for his science. And he seemed on the doorstep of victory too, a decade in the making.
“I usually heard Sam before I saw him.” UNeMed’s Joe Runge said. “Sam’s boundless energy and optimism was infectious. He was a force of nature in perpetual motion”
His energy and enthusiasm never flagged. In fact, that enthusiasm was the dominant trait in any given room he entered.
“His passion and energy were obvious from the get-go and it was contagious,” said Matt Boehm, UNeMed’s Licensing Manager who worked with Sam for about eight years. “He had ups and downs and tough times, but he always stuck in there and kept going. There were times when it would have been easy for him to walk-away but he never did, and I admire him for that.”
Said Dixon: “We probably didn’t realize it while he was here, but Sam really was the cat’s pajamas.”
Visitation for Sam Sanderson will be held at St. Stephen the Martyr Catholic Church in Omaha on Friday, Aug. 11 at 5-7 p.m. Vigil begins at 7 p.m. Funeral services will also be at St. Stephen the Martyr at 10 a.m. on Saturday, Aug. 12.
















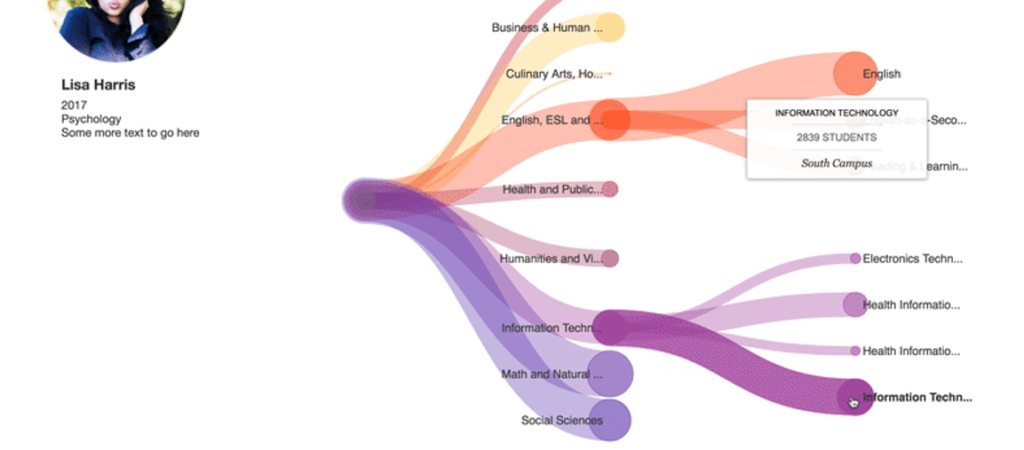
 I am now a Licensing Associate now at UNeMed Corporation, the technology transfer office at the University of Nebraska Medical Center. UNeMed gave me the opportunity to attend Association of University Technology Managers’ 2017 Annual Meeting in Hollywood, Fla. I noticed a stark difference in cultures between the two conferences.
I am now a Licensing Associate now at UNeMed Corporation, the technology transfer office at the University of Nebraska Medical Center. UNeMed gave me the opportunity to attend Association of University Technology Managers’ 2017 Annual Meeting in Hollywood, Fla. I noticed a stark difference in cultures between the two conferences.