 OMAHA, Neb. (Oct. 3, 2014)—The public will get the rare chance for a close and personal look at innovative technologies emerging from the research labs at the University of Nebraska Medical Center.
OMAHA, Neb. (Oct. 3, 2014)—The public will get the rare chance for a close and personal look at innovative technologies emerging from the research labs at the University of Nebraska Medical Center.
Sponsored by UNeMed Corporation, the second annual UNMC Technology Demonstration Day will be held Monday, Oct. 7, at 2:30 p.m. in the Durham Research Center I auditorium. UNeMed is the technology transfer office that helps UNMC’s groundbreaking research go beyond the laboratory.
Demonstration Day is a free and open event that will feature about six technologies (see below) developed at UNMC. Most of the featured innovations are either the cornerstone of a new local startup, or have been licensed by an existing company for further development. Inventors, startup CEOs or their representatives will deliver a short, 10-minute presentation, followed by a brief question and answer forum. UNeMed will then host a reception in the atrium with complimentary food and refreshments.
Space is limited, but a seat for UNMC Technology Demonstration Day can be reserved at https://unmcdemoday14.eventbrite.com.
UNMC employees and students who register online will also be automatically entered for a chance to win a free iPad, which will be announced at the Innovations Awards ceremony.
Innovation Week kicks off with an open house Monday, Oct. 7, at 9 a.m. in the DRC I atrium, where visitors can register another entry for the free iPad drawing, and pick up a free UNeMed T-shirt and other goodies. UNeMed will also offer free beverages at the open house.
UNeMed will host a seminar about building better collaborations between academia and industrial partners on Tuesday, Oct. 21 beginning at 10 a.m. UNMC personnel who attend the seminar will also gain an additional entry for the iPad drawing.
An on-campus scavenger hunt will wrap up Wednesday, awarding prizes to the winners who accumulates the most points. Go to the UNeMed’s Innovation Week webpage for additional details on the scavenger hunt.
Innovation Week culminates on Thursday, Oct. 23 with the UNMC Research Innovation Awards Ceremony and Reception beginning at 4 p.m. At the conclusion of the awards, UNeMed will draw for the free iPad 2. The winner must be present to claim the prize or a new name will be drawn.
The event is free, but space is limited, so reserve a seat for the Innovation Awards at https://iw2014.eventbrite.com.
Shared data needs middleman — Labpoint president and founder John Glock will discuss his Omaha startup’s climb from an idea to a working web solution that help labs, clinics and hospitals increase efficiency by improving their ability to share critical information despite using different hardware and software platforms. Labpoint was created in 2007, born from an idea Glock had while working as an information technology manager at UNMC’s Nebraska Public Health Library.
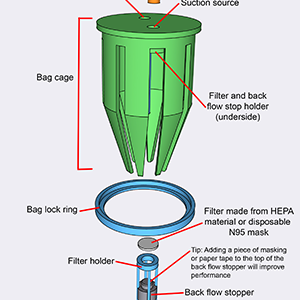
Laparoscopic simulator for higher skills, lower costs — Developing facilities for the purpose of training and maintain laparoscopic skills often requires a dedicated space and several thousands of dollars. A new, elegant system under development at UNMC can make virtually any open space a suitable training spot for laparoscopic tools at a small fraction of the cost. UNeMed’s Joe Runge will discuss this new training tool, and the clinical needs for cost-cutting innovations.
Detecting problems before the symptoms appear — The third-leading cause of death in the United States COPD, or chronic obstructive pulmonary disease, can lead to sudden and life-threatening exacerbations—a flare-up of symptoms that often result in hospitalization and an acceleration in the loss of lung function. Patients suffering from COPD must remain vigilant for the earliest signs of an exacerbation, but remarkable research from the biomechanics facility at the University of Nebraska-Omaha, have devised a platform that detect the earliest sign of impending trouble, long before a patient ever notices any of the traditional warning signs. Researcher Jenna Yentes, PhD, will discuss a the natural biorhythms in the human system and how they can tell us what’s wrong before we even know there’s a problem.
A better blood test for heart disease — Among the modern medical mysteries has been how a person with all outward appearances of health and youth die from a sudden heart attack. Finding those people at risk for the most dangerous forms of heart and artery disease could be as simple a new blood test currently under development at UNMC. Researcher and practicing heart specialist Dan Anderson, M.D., PhD, will discuss all we know—and what we don’t—about heart disease, and how we might be able to better manage artery disease in the near future.
Reinventing the surgical mesh — Acera Surgical is a medical device startup, in St. Louis, Mo., specializing in the next generation of surgical materials. Its cornerstone product, CeraFix™ Dural Substitute, is an implantable biosynthetic material, or scaffold, for use in brain surgery. Acera Surgical recently licensed a new UNMC invention for producing three-dimensional nanofabricated materials and matrices. Acera President Matthew MacEwan will discuss the shortcomings of modern medical meshes, and how UNMC’s and Acera’s innovations are the next generation of surgical materials.
Improving the hemodialysis catheter — An interventional nephrologist at UNMC, Marius Florescu, M.D., designed a new catheter with the potential to eliminate expensive and risky procedures for patients undergoing hemodialysis—the process that filters a patient’s blood. One common complication is that the catheter through which the machine removes and replaces the blood will become blocked, requiring surgery to replace the catheter and radiological imaging to verify the repair. Chrysalis Medical is a new venture formed in San Jose, Calif., by veteran medical device professionals and will build the prototype for testing at UNMC. Chrysalis CEO Ron Allen, is expected to lead the discussion.